Cor Exaudientis
He whispers again, dragging the listening heart of the young nurse beside him to wherever his mind is, into that well of memory…
~Michael Ondaatje, The English Patient
I owe a debt of gratitude to middle school Latin. I could already pronounce and spell many words in the language of medical terminology when I started work in an equine specialty and emergency hospital in 2005. So much was new to me in medicine. I found the familiar in horsemanship and in language: her roots in the twins, Latin and Greek. There was comfort in the familiar.
With my Latin roots, it was easy to differentiate between the suffixes for various classes of drugs, and to position the x-ray cassette correctly to capture, say, the dorsolateral-palmaromedial oblique view of the carpus. I loved the rigor and the specificity of this work. But I hadn’t suspected the limitations of science and knowledge to be so acute. Or that I would learn to speak for the non-verbal, to reconcile with words; what I wasn’t prepared for was how little we could actually control.
* * *
Col.ic (n.): a sharp sudden pain in the stomach; from Medieval Latin colic passio “intestinal suffering.”
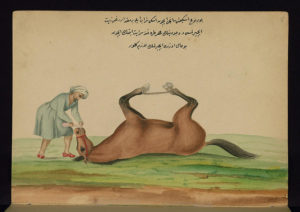
Healing a horse suffering from colic with old wine and olive oil (credit: Walters Art Museum, Public Domain Designation, CC0 1.0)
The horse has more unfixed organs than other large mammals, an advantage that allows speed—the full stretch into a gallop. With our modern practice of confining horses, their organs rebel against immobility by twisting among each other. Colic is a blanket term for the myriad gastrointestinal conditions that cause pain to a horse. It’s a clinical sign, not a disease.
Note: horses like to start dying after you’re asleep, preferably in snowstorms. In the hospital, you never say, “We haven’t treated a colic in a while” unless you want to guarantee a 3 a.m. page. My pager would shriek on the bedside table. I’d shake off the groggy and call into the clinic’s back line. The intern would answer, and say just one word: “Colic.” Colic is a four-letter word. I’d drive north to take my place on the surgery team.
Some colics are medically managed, and others surgically. Colic surgery requires anesthetic induction, a ventral incision, dorsal recumbency: so much Latin to describe what happens when a surgeon, an intern, and two technicians undertake the opening of a horse’s abdomen while his caretakers cry, pray—stand at the crossroads—in the conference room. Maybe the patient had an intussusception, a glorious word from the Latin intus (within) + suscipere (to take up), that particular obstruction when a bit of intestine slips back along the length before it. I controlled the anesthetic chart, its matrix of symbols and codes representing the elements of the horse’s life, his heart and lungs and blood.
In recovery, I transcribed: the surgeon might order 9600 milligrams of trimethoprim sulfa given orally every twelve hours; I wrote on the chart, 10 x SMZ 960mg PO q12h. I also translated: I’d read on the chart, TPR WNL, BAR, APP^; I’d say to the horse’s caretaker, “He looks good today, bright, no fever, even ate some bran mash this morning!” I wrote codes and crosschecked doses, but this says little of the lives I cared for. I controlled language, interpreted code to find life. The charting, the terminology, is where we chronicled our influence.
* * *
Uni.lat.er.al (adj.): occurring on one side; from Latin unus “one” and lateralis “side”
Hy.dro.ne.phro.sis (n.): cystic distension of the kidney caused by the accumulation of urine; from Greek hydro “water” and nephros “kidney.”
Ure.ter.o.cele (n.): cystic dilation of the lower part of a ureter into the bladder; New Latin from Greek and Latin urina “urine” and –cele “hernia.”

Arthur, when we met (credit: Katelyn Keating)
I met my dog, Arthur, in 2012, a few hours before he was scheduled to be euthanized. He was tied in the corner of the treatment room, where large dogs were most comfortable at the emergency vet practice where I worked in British Columbia. He’d had diarrhea for a few days. In the course of working up the case, the veterinarians inadvertently discovered Arthur’s congenital unilateral hydronephrosis with concurrent ureterocele. He needed major surgery, and his family said no: they chose to euthanize. I looked into this dog’s eyes and I said no.
I contacted my friend at a non-profit pet adoption group that regularly managed medical-necessity rescue pets, who convinced the family to surrender Arthur—to give him a chance at life. The charity funded the surgery to remove his atrophied kidney and distended ureter. I took him home to foster during his recovery. The term is “foster-fail,” for those pets who go into foster care and end up adopted by the foster parent. I have three foster-fails. As care provider and parent, I wrote both objective and subjective notes in his medical chart.
Objectivity and subjectivity require different languages: code switching. His objective notes read: TP WNL (temperature and pulse within normal limits) R ^ 60bpm (respiration elevated to sixty breaths per minute) QAR (quiet, alert, responsive) CRT <2 (capillary refill time less than two seconds). In his subjective notes I wrote, “Arthur wagged his tail and lifted his head. He’s got some pain, but he’s happy to see me.” Medical charting has a form and a creativity that speaks to my own balance of art and science, my brain’s overlapping hemispheres. I’m privileged to know both correct terminology and descriptive language to tell the story of a recovery.
* * *
De.men.tia (n.): a mental illness that causes someone to be unable to think clearly or to understand what is real and what is not real; from Latin demens “mad” and mens “mind.”
My dog Keegan’s dementia was different than my grandmother’s vascular dementia. At the Christmas gathering, Grandma patted my hand. She said, “Katy? How are you? How is school?” I answered, shouting past her deafness. Five minutes later she asked, “Katy? How are you? How is school?”
There was no facility to keep Keegan safe, like Grandma’s apartment with nurses on call. He lived with me, where he’d been since I was sixteen—half my life. Keegan was my soul. He’d been through all my changes with me.
His last year saw him diminished by Canine Cognitive Dysfunction—doggy dementia. He paced next to my bed at night, huffing and whining near my face. At the door leading outside he stood by the hinges. Once outside, he knew neither why, nor what to do. There is a drug for humans with Parkinson’s Disease that happens to work in some dementia dogs. It worked for Keegan and gave us one last year.
The day after he died, I wrote:

Canoeing Lake Campbell (credit: Katelyn Keating)
“I don’t remember who I was before him–I was no one, I was a child. Our lives were completely intertwined. I have never been sad without also being angry, and I don’t know how it works. I have nothing to be angry about. He lived a long and extraordinary life. He climbed mountains and canoed rivers and battled disease. There are hundreds of people whose lives have been touched by him. Most dogs never leave their block. Keegan saw the world and made his mark upon it.”
I don’t remember writing this, yet here it is, in a document titled, “A Life Less Ordinary,” dated March 31, 2009. I was in my fifth year of veterinary medicine, but would not call myself a writer for many more years. Here I was making writing inherent to my experience with death: writing life against death.
* * *
At December’s MFA residency at AULA, we learned about Narrative Medicine, a burgeoning interdisciplinary field described as “a model for humane and effective medical practice.” I took part in a workshop with Phillip Mitchell, who was interviewed with Emily Rapp Black (Still Point of the Turning World) and Juliet McMullin (The Healthy Ancestor: Embodied Inequalities and the Revitalization of Native Hawaiian Health) in the Lunch Ticket Summer/Fall 2016 issue. Founder of NarrativeCare, Mitchell leads writing workshops for caregivers as “continuing education that deepens relationships through the power of story.” He taught us by example:
Phillip first establishes a safe space, then guides a close reading of an excerpt from literature, in our case, the first few pages of The English Patient. He encourages the workshop to notice visceral, sensory details in the language. Then the group writes to a prompt. He usually leads workshops for health professionals who want to enhance their narrative skills, to learn fluency in empathy through storytelling, to create patient-centered practice by understanding more fully their patients’ stories. In December, we were a group of writers.
Our prompt was to write about “a room of caring.” We were undone in our language. In that safe space we translated, transcribed, interpreted. I came equipped with medicine and language. All I could control was words. This is what I wrote, transcribed from my notebook:
“It is my last night with you warm, in my bed. For 16 years, we have touched almost everyday. After tomorrow, I will feel you in the cool steel of an urn. Tonight, I set an alarm, every 2 hours, though I will not sleep, to remind me to keep your catheter patent, plunge 2 or 3ccs of heparinized saline into your arm leg. This will make it easier tomorrow. I will hold you close all night, worship your hair, take clippings of the amber curls, smell your feet, thankfully the same smell in every terrier’s feet—how else to live with this forever? In this rented apartment, this tiny bedroom, I will love all of you one more time. Your ghost will only visit me once. I will move to another country.”
* * *

Strait of Juan de Fuca from Keegan Hill (credit: Katelyn Keating)
I wanted Keegan to go out with dignity, on a good day. When enough of his medical conditions were irreversible, at the start of a decline with only one possible ending, we parted. He had stopped eating, and so he spent his second-to-last night on IV fluids in my hospital, tied in the same spot where I would later meet Arthur. Keegan didn’t bounce back.
We left his catheter in his leg for his final day and went to the park. Among the March daffodils, Keegan stood, looking out across the calm, blue-black expanse of ocean to where the Olympic Mountains of our home country rose on the other side. In our sixteenth year of us, we spent one last night together. A veterinarian friend came the next day to our verandah, in the sun and breeze, and put Keegan to rest.
* * *
Eu.tha.na.sia (n.): the act or practice of killing someone who is very sick or injured in order to prevent any more suffering; from Greek euthanatos “easy death.”
Keegan’s death was easy, and the hardest thing in the world. His suffering was gone, leaving mine in its stead. Now I write, and rewrite the same stories. Stories of animal life and animal death. My comfort in the familiarity of language—of Latin roots, of coding and subjective and objective language, of medical terminology—only holds me so far. My practice is to ease suffering with language. To love and write and remember. There is so little else I can control.
Katelyn believes the Tolkien mantra, “Not all those who wander are lost.” She also concurs with Agent Mulder regarding the location of the truth. She mixes metaphors. Hailing from New England, Katelyn lives in St. Augustine, Florida with her husband, two dogs, three cats, and several of her parents. She is an MFA student in creative writing at AULA. She serves on Lunch Ticket as the fifth Editor-in-Chief, having worked on prior issues as a staff blogger and Editor of Creative Nonfiction and the Diana Woods Memorial Award. Follow her @katelyn_keating.